Spurling’s Test
Spurling’s Test (also called the Foraminal Compression Test) is a clinical orthopedic assessment that helps diagnose cervical radiculopathy (compression or irritation of a nerve root in the neck) leading to radiating arm pain, numbness, or weakness. The test purposefully narrows the intervertebral foramen (nerve exit space), provoking symptoms if a nerve is compressed.
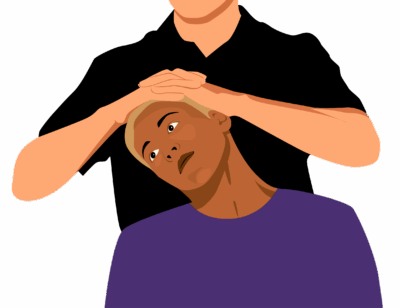
How the Test is Performed
-
Client position: Seated, relaxed, and upright.
-
The examiner gently extends, rotates, and laterally flexes (side-bends) the cervical spine toward the symptomatic side.
-
Axial compression is then applied through the top of the head (downward pressure) to further narrow the foramen.
-
The test is positive if:
-
The client’s usual arm pain, numbness, tingling, or weakness is reproduced in the affected dermatome (nerve distribution).
-
Neck pain alone is less specific for a positive test.
-
Clinical Significance
-
A positive Spurling’s Test strongly suggests cervical nerve root compression (radiculopathy) commonly due to disc herniation, spondylosis, foraminal stenosis, or facet arthropathy.
-
The test has high specificity (up to 95%)—a positive test is reliable for diagnosis.
-
Sensitivity is moderate, meaning a negative test does not rule out cervical radiculopathy; other signs and imaging may still be needed.
Assessment
-
Use Spurling’s Test for clients with neck pain plus radiating arm symptoms (pain, numbness, tingling, weakness), especially if worsened by head movement.
-
Document reproduction of symptoms and side tested. If the arm symptoms extend past the elbow, this supports diagnosis and tracks response to care.
-
Avoid repeated or forceful provocation, and do not use with clients who have known cervical instability, fracture, severe osteoporosis, or recent surgery.
Treatment
-
If positive:
-
Avoid deep tissue, intense cervical mobilization, or traction techniques that might further compress the nerve root.
-
Focus on gentle, pain-reducing soft tissue work for cervical, shoulder, and upper back muscles.
-
Educate clients about safe head/neck positions, posture, and gentle neural mobility work only if cleared by a supervising provider.
-
Refer for further medical/physio evaluation (and imaging as needed) if severe pain, progressive weakness, or unrelenting neurological symptoms are present.
-
Safety and Referral
-
Any new or worsening motor symptoms, sensory loss, or loss of bladder/bowel control warrants urgent referral.
-
Collaboration with physiotherapy, neurology, or orthopedic care is optimal for comprehensive management of true cervical radiculopathy.