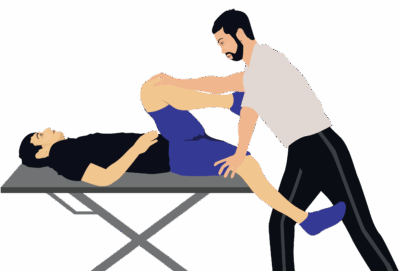
Gaenslen’s Test
Gaenslen’s Test is an orthopedic provocation maneuver used to assess dysfunction or pain in the sacroiliac joint (SIJ), though it may also stress the hip joint, pubic symphysis, or, less commonly, lumbar nerve roots. The test is designed to create torsional (shearing) forces across the pelvis and SIJs to reproduce symptoms in clients suspected to have SI dysfunction, especially in the context of low back, pelvic, or buttock pain.
How the Test is Performed
-
Client position: Supine at the edge of the treatment table.
-
The non-tested (contralateral) leg is maximally flexed, with the knee drawn toward the chest and held by the client or therapist.
-
The tested side leg (ipsilateral) hangs off the edge of the table in hyperextension at the hip.
-
The examiner applies downward pressure to the hanging leg (hip extension) while maintaining flexion force through the flexed leg, creating opposing shearing/torsional forces through the pelvis and SIJ.
-
A positive test: Reproduction of familiar SI region pain (buttock/low back), or sometimes pain in the groin or anterior hip on the extended side.
Clinical Significance
-
Positive Gaenslen’s Test indicates likely SI joint dysfunction, pain, or inflammation.
-
The test may also elicit pain in cases of pubic symphysis instability, hip pathology, or nerve root involvement (especially L4).
-
Used as part of an SIJ pain provocation test cluster—no single SIJ test is fully diagnostic; several provocation tests and a thorough history are recommended for accuracy.
-
Sensitivity and specificity vary; best diagnostic value when combined with other tests.
Assessment
-
Use Gaenslen’s Test in clients with unexplained low back, pelvic, or buttock pain or suspected SIJ/hip dysfunction.
-
Document the location and distribution of symptoms and which positions reproduce pain.
-
Always assess both sides for full comparison.
Treatment
-
If positive:
-
Avoid aggressive mobilizations, direct deep tissue, or high-velocity techniques over the SIJ or directly over the pelvis.
-
Focus therapy on gentle soft tissue and myofascial techniques to low back, gluteals, and pelvic stabilizers, as well as pain-modifying and stability-focused approaches.
-
Educate clients about postural correction, pelvic stability, and strategies to avoid excessive SIJ shearing (e.g., asymmetric lifting, prolonged single-leg activities).
-
Safety and Referral
-
Refer for further assessment (imaging, specialist) if SIJ dysfunction is severe, persistent, associated with significant functional limitation, or accompanied by red flag symptoms.
-
Collaborate with physiotherapists or orthopedic specialists for comprehensive management or complex cases.