Trendelenburg Sign
The Trendelenburg Sign is a simple orthopedic assessment used to evaluate the strength and function of the hip abductor muscles, especially the gluteus medius and minimus, and to assess for hip joint stability during single-leg stance. It is widely used for identifying hip abductor weakness, neuromuscular imbalance, and altered gait mechanics.
How the Test is Performed
-
Client position: Standing, feet hip-width apart, holding onto a stable surface if needed.
-
The client is instructed to lift one foot off the ground (stand on one leg) and maintain this position for about 30 seconds.
-
The therapist stands behind and observes the pelvic position, especially at the waistline or posterior superior iliac spine (PSIS).
-
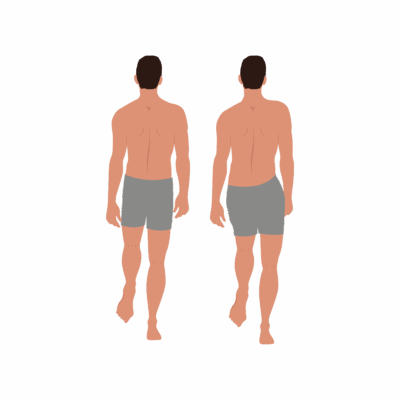
A negative test: The pelvis remains level or slightly rises on the lifted leg side, indicating adequate hip abductor strength. (Client on the left).
-
A positive Trendelenburg sign: The pelvis drops on the non-stance (lifted) side, indicating weakness or poor neuromuscular control of the hip abductors on the stance leg. (Client on the right).
Clinical Significance
-
A positive test suggests:
-
Weakness of the gluteus medius/minimus (hip abductors) on the stance leg.
-
Superior gluteal nerve dysfunction, hip joint pathology (e.g., arthritis, labral tears), gluteal tendinopathy, or poor neuromuscular control.
-
Possible leg length discrepancy or compensatory gait strategies, such as lateral trunk lean (compensated Trendelenburg).
-
-
Commonly seen in clients with hip pain, gait asymmetry, post-hip surgery, and certain lumbar/pelvic stability conditions.
Assessment
-
Use the test for clients with hip, pelvic, or lateral thigh pain, gait or balance issues, or suspected pelvic/hip instability.
-
Document whether there is pelvic drop, trunk compensation, balance loss, or pain, and which side(s) are affected for planning and communication.
Treatment
-
If positive:
-
Avoid aggressive, repetitive, or deep manual therapy over painful or unstable hip regions—work gently with soft tissue techniques, myofascial release, and address compensatory tightness in lateral trunk and lower limb.
-
Incorporate pelvic and hip stabilization work, education on safe gait mechanics, posture, and progressive gluteal strengthening.
-
Support functional movement retraining and home exercise as appropriate, collaborating with physiotherapists or trainers if needed.
-
-
If negative, reinforce maintenance of hip stability and integrated movement.
Safety and Referral
-
Refer to a physician or physiotherapist for severe or progressive weakness, unresolving hip pain, or suspicion of joint or nerve pathology.
-
Use the Trendelenburg Test results alongside other functional assessments for comprehensive care and monitoring.