Valgus Stress Test (Knee)
The Valgus Stress Test is a clinical orthopedic maneuver used to assess the integrity of the medial collateral ligament (MCL) of the knee. It is a fundamental test for identifying MCL sprains and medial knee instability, but can also help evaluate the overall stability of the medial knee joint complex.
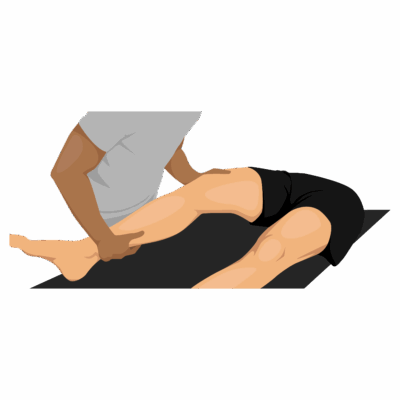
How the Test is Performed
-
Client position: Supine (lying on the back), legs relaxed.
-
The examiner stabilizes the thigh (femur) with one hand and holds the lower leg (ankle or foot) with the other.
-
A valgus (outward) force is applied to the knee—meaning the lower leg is gently pushed laterally (away from midline) while the thigh is stabilized, stressing the medial (inside) aspect of the knee.
-
The test is performed in two positions:
-
Knee fully extended (0°): Assesses major medial and cruciate ligament injury.
-
Knee flexed 20–30°: Specifically isolates MCL integrity since the cruciate ligaments are less taut.
-
-
A positive test: Increased medial joint gapping or pain compared with the unaffected leg, indicating MCL sprain/tear or medial capsule instability.
Clinical Significance
-
Positive at 20–30° flexion only: Suggests isolated MCL injury.
-
Positive at both 0° and 30°: May indicate combined MCL and cruciate/capsular ligament injury.
-
Sensitivity is high (up to 86%); best used in context with the full knee assessment and injury history.
Assessment
-
Use the Valgus Stress Test for clients reporting medial knee pain, instability, or history of trauma (direct blow to outer knee, twisting injury, etc.).
-
Always document degree of laxity, pain, and compare with the contralateral knee for clear records and referral.
Treatment
-
If positive:
-
Avoid deep tissue work or aggressive massage/manual therapy over the medial knee, especially in the acute or unstable phase.
-
Focus on gentle soft tissue work to the surrounding musculature (adductors, quadriceps, hamstrings, gastrocs), swelling and pain management techniques, and gradual stability work.
-
Educate clients regarding activity modification (avoid lateral stress, pivoting, or high-impact activity) until cleared by a healthcare provider.
-
-
Monitor healing and coordinate with physiotherapists or orthopedic teams for structured rehabilitation and progression.
Safety and Referral
-
Refer for further medical imaging or orthopedic assessment if instability is marked, acute trauma is suspected, or function is severely impaired.
-
Consider using test findings alongside other orthopedic assessments for comprehensive care.