Functional Leg Length Test
The Leg Length Test is a clinical assessment used to determine leg length discrepancy (LLD)—a condition where one leg is shorter than the other, either due to true bony difference (true/anatomic LLD) or due to biomechanical/postural causes (functional LLD). Identifying and understanding LLD is crucial for managing pain, posture, and gait issues in the lower body and spine.
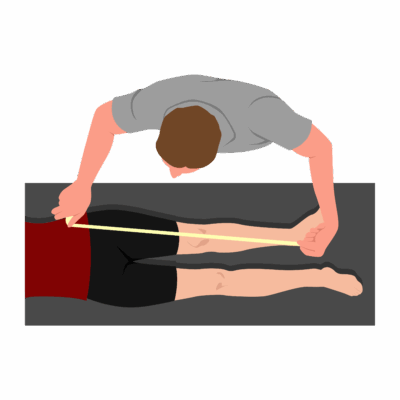
How the Test is Performed
Direct Method (Tape Measure)
-
Client position: Supine, pelvis level.
-
Measurement is taken from a bony pelvic landmark (usually anterior superior iliac spine [ASIS]) to the medial malleolus (inner ankle bone) on each leg.
-
Differences of more than 5 mm are considered clinically significant, but this method is subject to error from pelvic/limb misalignment and examiner variability.
Indirect (Block) Method
-
Client position: Standing upright.
-
Blocks of known thickness are placed under the shorter limb until the iliac crests or pelvis are level, as assessed by palpation.
-
The amount of lift required to level the pelvis equals the observed functional or true discrepancy.
-
This block test has the best clinical reliability and is recommended over tape measurements for most clinical purposes.
Clinical Significance
-
Functional LLD: Apparent—caused by pelvic tilt, joint contracture, or asymmetrical muscle tightness or postural habits.
-
Even a small LLD can affect gait, posture, and load distribution, potentially leading to back, hip, or lower limb pain.
-
Identifying the type and degree of LLD is key for targeting treatment.
Assessment
-
Assess for LLD in clients with:
-
Pelvic, back, hip, knee, or lower extremity pain
-
Gait differences or symmetrical postural complaints.
-
-
Document the test method used, findings from both the direct and block methods, and any associated compensations or postural adaptations observed.
-
Be aware of sources of error, especially with tape measure technique (ensure careful anatomical landmarking and repeat measurements for reliability).
Treatment
-
For functional LLD:
-
Focus on manual therapy and corrective exercise to address muscle imbalances, pelvic alignment, and postural patterns.
-
Reassess frequently as soft tissue and postural changes can alter functional discrepancy.
-
-
Educate clients on foot wear, ergonomics, gait retraining, and home strategies to minimize the impact of LLD.
Safety and Referral
-
Refer for imaging or to a specialist if there is significant, unexplained, or symptomatic discrepancy, or when conservative strategies do not resolve complaints.
-
Monitor client progress and coordinate care with physiotherapists or orthotists as appropriate.